- Arabic Corner
- Audio
- Bible Study
- Coptic Reader
- Children's Corner
- Deacons
- Evangelism & Apologetics
- Evangelism Pamphlets
- Interesting Facts
- Literature
- Pigori Productions
- Priests Corner
- Questions & Answers
- Reading Recommended
- Saintly Studies
- Servants Guide
- Sunday School Curriculum
- Sunday School Curriculum-Special Needs
- Youth Corner
Brain Death
![]() Print
|
Print
|
![]() Send to a friend
|
Send to a friend
|
![]() Bookmark
|
Tweet
|
Bookmark
|
Tweet
|
![]() Back
Back
Background: The matter of brain death is new to our Coptic Orthodox Church as it is new to our Egyptian culture.
Objective: To establish uniform understanding of the definition of brain death, coma state, persistent vegetative state, and to establish reasonable criteria for cessation of life support.
Future goals: (1) To spread the knowledge to our Church in Egypt, and to our Coptic Orthodox Church in all continents.
(2) To give some guidelines to our Holy Synod to make recommendation about brain death and withdrawal of life support.
Introduction:
The Neurologic Brain Death Syndrome is relatively new to us. Before the advent of high technology resuscitation, maintaining vital function in seriously neurologically injured patients was very impractical. Patients with massive head injuries or intracranial hemorrhage died at the scene or shortly after.
We owe our knowledge to French physicians who first described the clinical picture of brain death. In 1959, they called it coma dépassé. It was not until 1968, about 9 years later, that Americans started to realize the concept of brain death. It was in August 1968, nine months after the first heart transplant in the world that took place in South Africa. The Harvard Ad Hoc Committee on Irreversible Coma was the first in America to publish the clinical features of brain death.
Solid Statement:
The Harvard Committee stated that when treatment is stopped in a brain dead person, it is stopped not because therapy is futile (not useful), non beneficial, or burdensome, but because the patient is already dead.
Various clinical criteria that slightly differ from the Harvard studies were also developed in USA and abroad in the 1970s to 1980s. The President’s Committee for the Study of Ethical Problems in Medicine also established some criteria.
The criteria contained in the report consists of two components.
(1) Loss of both cerebral hemispheres and brain stem function.
(2) Irreversibility is established.
Requirements: In most states a neurologist or neurosurgeon is the one that declares brain death. It is widely accepted that brain death is defined as an individual with irreversible cessation of all functions of the entire brain including the brain stem.
(1) Cerebral functions are absent and there must be deep coma. Medical circumstances may require the use of confirmatory studies, an EEG (electroencephalogram), or blood flow studies.
(2) Brain stem functions are absent. The brain stem has the center for respiration (breathing).
Special Circumstances:
Peripheral nervous system and spinal cord reflexes may persist after death. For example, in the Lazarus phenomenon, after a patient is declared brain dead, some movement will occur and it has even been reported that the patient will sit up in bed. Often, the transplant surgeon faces this problem in the process of the transplant and becomes very anxious. However, the neurologist should inform the surgeon about this phenomenon.
Irreversibility:
a) The cause of coma is established and is sufficient to account for the loss of brain function.
b) The possibility of recovery of any brain function is excluded. The most common reversible conditions are: sedation, low temperature (hypothermia), and shock.
c) Cessation of all brain function persists for an appropriate amount of time. For example, 12 hours or 24 hours if anoxia/loss of oxygen to the brain.
Infants, neonates (new born), and children: Certain modification of the criteria should be considered. For example, longer period of observation in neonates (7 days to 2 months of age). It is advisable to observe neonates for 48 hours.
For infants 2 months to 12 months of age, it is advisable to observe for 24 hours.
If patient is less than 10 years of age, one of the two attendings confirming death must be a pediatric neurologist.
Harvard Criteria for brain death:
(1) Unresponsive coma
(2) Apnea
(3) Absence of cephalic reflexes
(4) Absence of spinal reflexes
(5) Flat EEG
(6) Persistence of condition for at least 24 hours
(7) Absence of drug intoxication or hypothermia
Statement by Plum and Posner in diagnosis of stupor and coma:
There is substantial evidence from thousands of patients around the world that not a single person who fulfilled the criteria of brain death has maintained heart beat for more than a few days, no matter what treatment was delivered.
Brain death and cadaver organ transplant:
(1) Mandatory Criteria:
A. Coma of established cause
- No anesthetizing amount of toxins or therapeutic drugs. For example, Phenobarbital or Ativan.
Low temperature below 30ºC should be corrected as much as possible. - Irreversible structural disease or a known irreversible metabolic cause due to organ failure must be present.
- No cerebral function
- No brain stem reflexes
- Pupils must be fixed to light, dilated or mid position
- No corneal reflex - No response to ice water caloric test (50-100 mL in each ear)
-The circulation may be intact
-Purely spinal reflexes might be retained (e.g. Lazarus phenomenon) - No spontaneous breathing on apnea test
- Pupils must be fixed to light, dilated or mid position
A. EEG for 30 minutes shows absence of cerebral activity, flat nul, or isoelectric silence
B. Brain stem auditory reflexes or somatic evoked potential might be tested
C. No cerebral circulation on angiography examination
Why do we declare a person brain dead?
(1) To remove patient off ventilator (breathing machine)
(2) To donate his or her organ for organ transplants. Sometimes the family is pressured to give consent for organ donation. Take into consideration that organ donation cannot occur without the consent of the family. In many circumstances, if organ donation is not agreed upon by the family, declaration of brain death will be of much less value and there is no rush to remove the patient from the ventilator.
Should we remove our patient from the ventilator ("pull the plug") or leave him until he dies?
A patient who is brain dead will suffer cessation of heart beat (heart will stop) within days or rarely a week or so of the diagnosis. It means eventually sooner or later, ranging from 1 day to 7 days, the heart will stop with no recovery. If the patient during his lifetime or his family has consented to organ donation, it is acceptable at this point to pull the plug or take the patient off the ventilator.
If the family did not consent to organ donation, any way the heart will stop in a matter of hours or days.
Can we object to cerebral death due to religious reasons?
The states of New York and New Jersey changed their statute to accommodate religious objections. These amendments require physicians to honor these requests and to continue medical care despite evidence of the loss of brain function.
Dear Abouna, should we remove life-sustaining treatment for my father or mother if they are in a coma?
The American Academy of Neurology does not dictate withdrawal of life-sustaining treatment in prolonged comatose patients.
Dear Abouna, my father is in Egypt. I was told that he is mechanically dead. Is he dead or alive?
The term "mechanically dead" does not exist in the American literature. It is not an accurate description of his neurological status. Further evaluation should be done before declaring him brain dead.
Dear Abouna, what happens in different states in America and in Canada?
In general, the USA Determination of Death Act mandates irreversible cessation of all functions of the entire brain and brain stem and irreversibility.
Loss of whole brain function as determined by any physician has become legally justified in Canada. In 2000, the Canadian Neurocritical Care Group published guidelines for diagnosis of brain death that closely mirrors American Academy of Neurology guidelines. Virginia specifically calls for specialists in neuroscience. Florida mandates two physicians, one must be the treating physician, and the other must be a board eligible or board certified neurologist, neurosurgeon, pediatrician, internist, surgeon, or anesthesiologist. California, Alabama, Iowa, Louisiana, Florida, Virginia, and Kentucky require independent confirmation by another physician, but one physician determination is sufficient in most cases. In Alaska and Georgia, a registered nurse is the delegated authority to declare death but with subsequent certification by a physician in 24 hours.
Dear Abouna, what happens in the rest of the world?
In Central and South America, there are official guidelines. However, there is a lack of description of the apnea test. Confirmatory test are optional in the majority of surveyed countries. In Europe, there is a fairly uniform agreement regarding criteria for clinical evaluation of brain death. Eleven of 25 guidelines require a confirmatory test. In Hungary, certain conditions extend observation for 72 hours. In Turkey, a cardiologist, neurosurgeon, neurologist, or anesthesiologist examine the patient followed by confirmation tests. In the country of Georgia, 5 years of experience in neuroscience is required, but it is not required in Russia. In Africa, virtually all African countries are without legal provisions for organ transplant, so brain death criteria are difficult to obtain. Only Tunisia and South Africa have guidelines. In the Middle East, brain death criteria were approved by Pan-Islamic Council in Jordan in 1986 and in Mecca in 1988. However, official guidelines have not been drafted in many countries. In Israel, the team is two physicians and should exclude the treating physician. In Asia, Australia, and New Zealand, India, and Bangladesh there are major differences determining brain death. In Iran, 12, 24, 36 hours of observation by 3 physicians is recommended. In China, there are no legal criteria. Hong Kong closely reflects United Kingdom’s criteria. Japan has a unique feature of requiring a CT of the brain showing irreparable damage.
The first formal exam performed by 2 physicians after at least 4 hours have elapsed. The second exam performed 2 hours after the first exam. The exception is in primary hypoxia (low oxygen to the brain), in which the first exam should not be performed until 12 hours.
Dear Abouna, my father is unconscious. Is he in a coma or persistent vegetative state, or is he brain dead?
Minimally conscious state is a new term (MCS) introduced in 2002. It is a condition of severely altered consciousness or unconsciousness in which minimal but definite behavior evidence or environmental awareness is demonstrated. There is intermittent unequivocal evidence of consciousness demonstrated by attention, intention, and memory. This is in contrast to persistent vegetative state (PVS) in which there is no awareness of self, others, or the environment. MCS can recover.
It has been estimated that diagnostic error rates for MCS patients as persistent vegetative state may be as high as 30 to 40%.
Coma
Patients in a coma have complete failure of arousal system with no spontaneous eye opening and are unable to be awakened by application of vigorous sensory stimuli.
Persistent Vegetative State (PVS)
Persistent vegetative state is characterized by complete absence of behavioral evidence for self or environmental awareness. There is a preserved capacity of spontaneous or stimulus-induced arousal evident by sleep-wake cycles. They can posture or withdraw to noxious stimuli. Hearing: there is brief orientation to stimuli. Visual: there is brief visual fixation. Emotion: there is reflexive crying or smiling. Motor function: can occur with non-purposeful movement. Communication: none.
Unlike brain death, in which cerebral hemisphere and brain stem both undergo loss of their activity, the pathology of persistent vegetative state is often limited to cerebral function and only occasionally is there indication of damage to focal area in brain stem.
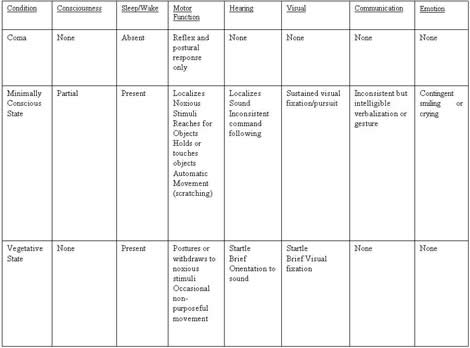
Chart adapted from Neurology Journal 58, 2002, page 350
Brain death made simple
Dear Abouna, what is brain death?
Brain death is the cessation of the functions of both cerebral functions and brain stem. Cerebrum is the top of the brain. The brain stem is the lower part of the brain that contains the respiratory center. So, if the respiratory center is damaged, the patient will die even if he is placed on a ventilator.
![]() Print
|
Print
|
![]() Send to a friend
|
Send to a friend
|
![]() Bookmark
|
Tweet
|
Bookmark
|
Tweet
|
![]() Back
Back